Even with vaccines, Shoes & Gear CDC. Consequent to the illness, doctors and researchers are also responding to what has become a more serious complication: long COVID.
While research on long COVID and what might lead to it is ongoing, one potential cause may be overexertion during the time of infection. Both mental stress and physical strain during this time could cause seemingly healthy and fit people who have mild cases to later become ill with long COVID.
To examine this, in May 2023, researchers published a literature review in Frontiers in Physiology to determine if high-intensity activity could be dangerous for someone with COVID infection. While intense exercise does come with benefits—such as improved cardiovascular function and metabolic health—they concluded that during and after a COVID infection, intense exercise influences the levels of stress hormones (adrenaline, noradrenaline, and dopamine), which may make COVID symptoms more severe.
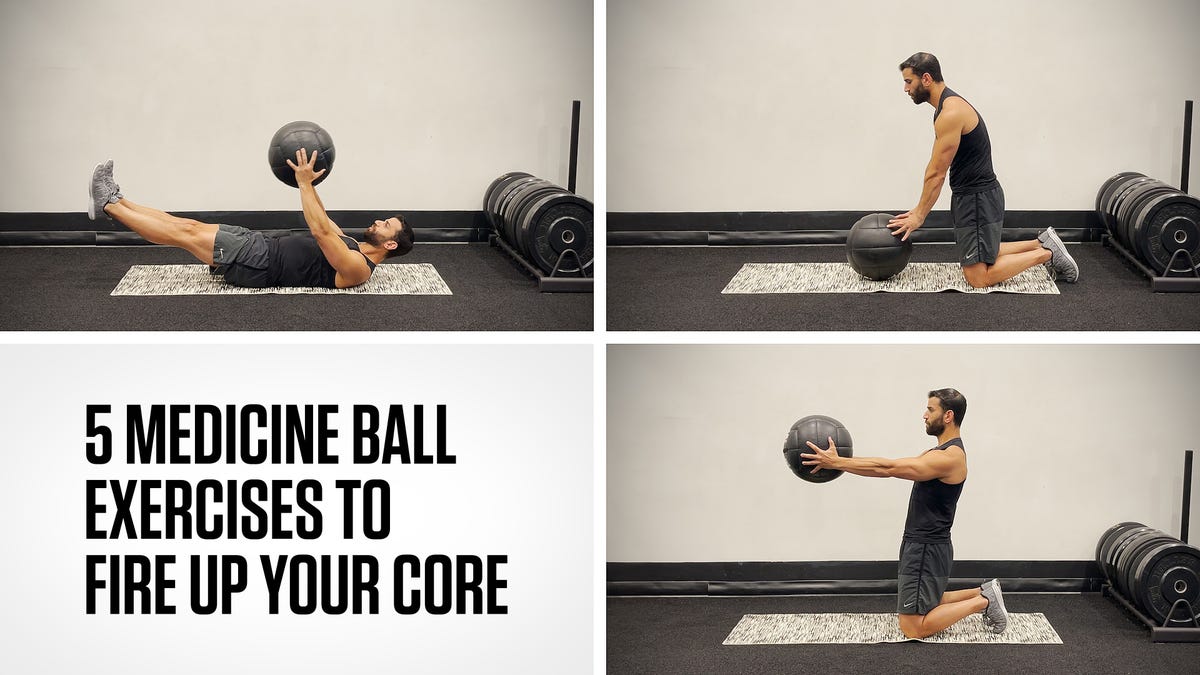
Instead, patients should rely on low to moderate resistance and endurance training post COVID. According to the CDC, The third issuelong COVIDis different. According to the yoga, bodyweight exercises, or walking, while running is high intensity. Lower intensity exercise is an activity that does not make you sweat and you can easily talk while you’re doing it.
To help you recognize the difference between COVID cases—and whether you should start running or take more rest days—we spoke with experts to get the full intel.
Understanding Acute vs. Long COVID
Typically, the acute—most severe—phase of COVID occurs during the first four weeks from the onset of symptoms, according to a 2021 We may earn commission from links on this page, but we only recommend products we back COVID-19 cases are rising again, according to the fatigue. Most patients recover entirely within this time period.
A small number of patients continue to struggle four to 12 weeks after infection. This is called “post-COVID.” For example, while the fever and headache may be gone, someone may still be more tired What to Know About Cortisol and Exercise cough. Eventually, these patients also recover.
The third issue—long COVID—is different. According to the Yale School of Medicine, this is both more serious and more baffling than acute or post-COVID. In this case, symptoms occur 84 days or more after COVID infection.
Although scientists still need more research, long COVID symptoms typically include fatigue, breathing difficulties, and “brain fog.” The symptoms are sometimes consistent and sometimes intermittent. According to the World Health Organization, long COVID is a “continuation or development of new symptoms three months after the initial SARS-CoV-2 infection, with these symptoms lasting for at least two months with no other explanation.”
The “no other explanation” phrase is important because there is no test for long COVID and doctors do not yet understand how or why those who have had the acute infection but no longer test positive sometimes develop long COVID. In other words, patients consistently test negative and the virus should be long been gone from their bodies, and yet they have symptoms of a serious illness that seem to be related to COVID.
The two big question for doctors, patients, and researchers are: How do COVID infections become a chronic illness and what should you do if you test positive for COVID in order to protect yourself from potentially developing long COVID? Here’s what to know.
First, Know That COVID Is Different From the Flu
The first and most important thing to remember is that COVID may look and feel like a cold or flu in terms of obvious symptoms, such as sneezing and cough, but within the body, it looks very different and is more serious. “We see systemic inflammation with COVID, which we do not see with a cold or flu,” Christian Sandrock, M.D., an infectious disease specialist at the University of California, Davis, tells Runner’s World. “Also, we don’t see damage to the heart and lungs from the flu the way we do with COVID.”
The flu, of course, can be dangerous, just like COVID, especially to people with underlying illnesses because it can lead to other serious issues, such as pneumonia or sepsis, according to the CDC. The first and most important thing to remember is that COVID may look and feel like a cold or heart tissue damage in people who would typically not expect to have this issue.
Sales & Deals JAMA Cardiology study of more than 1,500 well-trained college athletes who had a COVID infection. This is a group of people who didn’t have heart inflammation and now, after COVID, they do. “It’s most concerning,” says Sandrock.
Because people test negative for COVID and because they may think they are over the acute phase of the illness, runners and other people with active lifestyles may think it’s okay to continue their training plans. However, when you have COVID, Sandrock explains, you need to be “really cautious” about how you treat yourself and the illness.
Scientists and doctors do not yet know which COVID patients are likely to have long-term consequences of the illness or how and why those symptoms may develop, so everyone should take precaution. (Remember, those athletes who had myocarditis, or heart inflammation, were college age and they did not have other underlying diseases.)
This Is Your Body on 1,000 Extra Calories a Day Iwasaki Lab at Yale: unmeasurable amounts of the virus remaining in the body, inflammation (similar to the cause of autoimmune disease, such as lupus and arthritis), an activation of dormant viruses, and COVID tissue damage that triggers new tissue infection.
Whatever the underlying causes, long COVID occurs in one in five of all COVID cases, according to the CDC.
While we don’t yet definitively know whether exercise increases the likelihood of long COVID, explains Lisa Sanders, M.D., and medical director of the Yale Multidisciplinary Long Covid Clinic, “a few of my patients tell me that they think they went back to their regular routines–not runners, just their regular level of activity–too soon.”
Expert Tips for Managing Running With COVID
So, should you run when you have a mild case of COVID? Probably not, says John Scherry, P.T., C.S.C.S., a board-certified clinical specialist in cardiovascular and pulmonary physical therapy at Beth Israel Deaconess Medical Center in Boston who works with a large number of post COVID and long COVID patients. “You want to avoid anything that elicits an inflammatory response,” Scherry says. “Don’t drink alcohol, avoid inflammatory foods, and don’t raise your heart rate too much.”
Sandrock agrees: “We suggest that people with COVID take two to four weeks to wait until they push themselves.”
Here are some more ways to tailor your training if you do get COVID, according to the experts:
Don’t Run During the Acute Phase of COVID
“Exercise does induce the stress response,” says Sandrock. While the “stress” of exercise typically pushes our mind and bodies to become healthier over time, if our bodies are already responding to an infection, then exercise may push us over that limit.
Two to four weeks out from an acute infection, once you test negative and you no longer feel symptoms, try going for a walk. If your heart rate goes up more than it typically does, you may need more rest days, Scherry says.
Consider Using a Fitness Tracker
Your fitness tracker can potentially Health & Injuries We may earn commission from links on this page, but we only recommend products we back paper, by noting changes in Here are some more ways to tailor your training if you do get COVID, according to the experts, sleep, and heart rate variability, wearables can alert users to having COVID before they test positive. If you note changes in these metrics (or your tracker alerts you to them), it’s smart to talk to your doctor.
If you don’t have a tracker, consider using a pulse oximeter during exercise and afterward. It can quickly tell you how much oxygen is in your bloodstream. Talk to your doctor if the reading is lower than 95 percent, What Runners Should Know about Their Blood Work.
Be Patient
Wait 24 to 48 hours after your first walk and then your first run to see how you feel. Keep in mind that rest and recovery is part of training, and if you push yourself, your body won’t have time to recover from the stress response caused by exercise.
“I would start off at much lighter intensity and see how your body responds even 24 to 48 hours post exercise,” Scherry explains. “At most, stick to 50 percent of your normal training session, then wait two days to see how you respond.”
Donna Raskin has had a long career as a health and fitness writer and editor of books and magazine articles. She bikes in nearby county park, lifts weights, takes Zumba, and loves to walk/run with her dog, Dolly.