Studies have shown that roughly half of recreational runners will suffer an injury during their training year, with the knee as the most common site of injury. Kneecap pain can be debilitating and frustrating, and the prolonged pain and dysfunction lead many to abandon or limit running. Kneecap pain is sometimes referred to as runner’s knee, chondromalacia patella or patellofemoral pain.
The knee joint is comprised of three bones: the tibia, the femur and the kneecap or patella. The patellofemoral joint generally refers to the kneecap and its underlying groove or trochlea, with which it articulates. The four muscles of the quadriceps share a common attachment on the patella. The kneecap plays an important role as it lengthens the lever arm of the muscles and tendons of the quad and protects the front of the knee from direct trauma. Because it’s subjected to forces up to 8 times bodyweight with running and jumping, the cartilage underneath the kneecap is among the thickest in the body. This cartilage is a natural shock absorber and protects the bony surfaces of the joint from stress. While cartilage doesn’t have any nerve supply, the underlying bone is highly innervated and becomes vulnerable when no longer protected by the padding of the cartilage.
Sports medicine professionals identify patellofemoral pain as constituting a quarter of the injuries to the knee. Research in the British Journal of Sports Medicine suggests that women are more commonly affected than men, likely because of anatomic factors that place more stress on the kneecap. While researchers readily identify the prevalence of the condition, they aren’t as quick to agree on the cause and proper treatment of the injury, as it likely stems from multiple factors. Tracking of the kneecap is influenced by many sources. Imbalance in any of these forces due to weakness or tightness can lead to improper tracking and overload of the cartilage under the kneecap.
We may earn commission from links on this page, but we only recommend products we back
Runners will usually experience a gradual onset of pain around the edge or underneath the kneecap during or after running. Other than running, this soreness can be aggravated by squatting, descending stairs or hills, and sitting for long periods. Occasionally mild swelling around the kneecap might be present, but not to the extent of swelling present after more traumatic knee injury. Frequently, there’s an increase in the popping and cracking of the kneecap when bending and straightening the knee.
The most commonly accepted theory is that increased stress to the kneecap results in wear to the underlying cartilage. There are several biomechanical and anatomic factors that have been linked to this increased pressure and have been implicated in the scientific literature in the development of kneecap pain. Of the anatomic factors, an increase in the angle of the hip and knee, or Q-angle, is frequently considered to heighten the risk of injury. Several factors, such as being “knock-kneed” or having a greater degree of foot pronation, can contribute to an increase in this angle. Functionally, weakness of the outer hip muscles leads to a greater degree of inward knee movement when walking or running.
Weak Quads
Researchers in the Clinical Journal of Sports Medicine propose that the most important biomechanical and anatomical factor is the balance of the medial and lateral quad muscles. It’s theorized that the medial stabilizer of the kneecap is overpowered by the lateral stabilizer, changing the tracking of the knee and possibly overloading the outside portion of the kneecap. Weakness of the medial stabilizer of the kneecap, part of the quad called the VMO, is believed to play an important role in the development of improper tracking and kneecap pain. While many researchers have thought that exclusively strengthening the VMO will lead to improved tracking of the kneecap and a reduction in pain, researchers have been unable to achieve pure isolated strengthening of the VMO with exercise.
Because those who suffer from chronic kneecap pain have decreased quad strength, importance should be placed on regaining overall quad muscle strength rather than trying to achieve complete isolation of the VMO. Sports medicine researchers in Finland validated this approach as they found that regaining quad strength predicted the most favorable results in those with chronic patellofemoral pain.
We may earn commission from links on this page, but we only recommend products we back
An equal number of scientific studies point to strengthening the outer hip muscles as the key factor in treating kneecap pain. Weakness of these outer hip muscles is suggested as a cause of increased inward movement of the knee when running. While recent research in the American Journal of Sports Medicine couldn’t establish hip muscle strength as a predisposing factor in developing kneecap pain, many studies have found hip muscle weakness in those who have the condition. It’s likely that the resulting hip weakness is present because pain and inflammation has led to disuse of the injured leg.
While current research seems to indicate that stretching plays a lesser role in treating kneecap pain, improving quad, hamstring and IT band flexibility has been shown to have a beneficial effect. Inflexibility in these muscles can influence normal movement of the kneecap and contribute to abnormal tracking.
Treatment
As many factors can lead to the development of kneecap pain, successful resolution of the condition should unite the treatments suggested in the medical journals: incorporating strengthening and stretching of the leg. For the treatment of kneecap pain, clinical and scientific evidence points to the importance of reconditioning the quads and outer hip muscles. With its direct attachment to the patella, the quad muscle plays a critical role in reducing the pressure on the kneecap when running. When strengthening the quads, exercises such as squats, wall sits and leg presses have proven most effective and safest. Additionally, addressing the strength of the outer hip muscles is important in controlling the inward motion of the knees when running.
When running results in kneecap pain, the first step of treatment should be a significant reduction or cessation of running. Trying to run through knee pain will generally only make the problem worse and delay recovery. Cross-training on the stationary bike can be used to maintain fitness while reconditioning the quad and leg. After the kneecap inflammation has resolved and the leg has been reconditioned, a running progression can be resumed.
Muscle tone, along with quad and leg strength, will be reduced when resuming training, the amount depending on the length of time since the onset of knee pain; therefore, exercises that are geared toward improving the muscle tone of the quad should be incorporated to begin the process of strengthening without putting undue stress on the kneecap. Exercises that use the quad with the knee straight, those that improve outer hip and hamstring strength, and very light strengthening on the leg press can be included in the early recovery period. As the inflammation improves, more advanced training, such as body weight squats, can be added to the strengthening program. Stretching and soft-tissue mobilization of the quads, hamstring and IT band should be included to address any potential inflexibility.
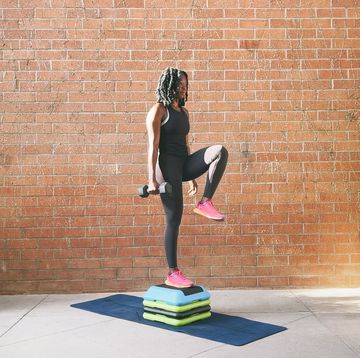
If several weeks of successful progressive strengthening is combined with a significant reduction of pain, additional cardiovascular training on the stair machine and elliptical can be added as a transition back to running. At this point, inclusion of functional pre-running drills is an important step in transitioning increased strength into improved running mechanics. These drills serve as a test and also train the leg to use the quads and hips to absorb the impact of running.
When the kneecap can tolerate a full strengthening and functional workout without any kneecap soreness or pain, running can be resumed, in a careful progression. As any sports medicine professional would advise, a runner recovering from injury shouldn’t quickly resume a former level of training without first building up mileage and volume over a one- to two-month period. The length of the transition period should directly correlate with the time off of running. For those who’ve not been able to run for three to six months, adding five minutes of running a week is recommended.
This program is not designed to be a substitute for a consultation with a trained sports medicine practitioner — if knee symptoms persist or there’s difficulty with the exercise program, a more individualized evaluation may be needed. Most are able to return to running after conservative treatment, but if kneecap pain persists, additional options do exist. Anti-inflammatories are often prescribed along with physical therapy. If all of these measures are unsuccessful, surgical options can include altering the tracking of the kneecap or addressing any problems with the cartilage.
RELATED ARTICLE: Shoes & Gear
A sports medicine professional, Ian McMahan focuses on science and endurance performance topics. He lives in Northern California and has raced every type of bicycle, using that as his reason to own as many bikes as possible.